View Products for Testosterone
All About Testosterone
Effects of Aging
Low Testosterone Signs and Symptoms
Psychological Symptoms
Screening Questionnaire
Testosterone Stimuli
Clomiphene Stimulation
The Power of Nutrition
Low Testosterone and Overall Health
The Easy Solution – Testosterone Replacement Therapy
The Goal of Therapy
What Experts are Saying
When Therapy is not Recommended
Forms of Therapy
References
The following is detailed information to help you better understand the problems and solutions associated with low testosterone. We have many different products to help with low testosterone and have referenced the better product to make it easier for you.
As noted elsewhere on this website, when discussing any organ system in the body, it is important to understand that organs do not work in isolation; everything works as a whole system. For example, influences such as diet, nutrition, exercise, trauma, immune and inflammatory imbalance, oxidative stress and energy production, gastrointestinal status, detoxification, musculoskeletal structures, other hormones and neurotransmitters, mind, spirit, emotions, and community, and genetic predisposition may affect testosterone levels. All these factors should be evaluated to return the testicles from a dysfunction state to normal function.
Figure 1 depicts the influence testosterone has on a man’s body.
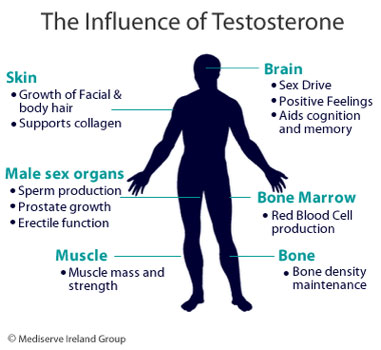
Figure 2 depicts the different types of testosterone. The entire circle is the total testosterone, the majority of which is bound tightly to sex hormone binding globulin (SHBG) and loosely bound to albumin. Only small amount (about 2%) is free. The tissues of the body only respond to the free portion, so it’s that portion that’s not bound. A small portion of the testosterone that is bound to albumin is available to participate in the tissue response. This is called the bioavailable testosterone.
The free and bioavailable testosterone will depend on the amount that’s bound to SHBG, therefore the more that’s bound, the less is free and the less is bound, the more that’s free. The normal range for SHBG is 20 to 60 nmol/L. If there is excess or low SHBG, healthcare professionals must ask why.
Effects of Aging
Aging, hyperthyroidism, Type 1 diabetes, alcoholism, smoking, caffeine and vegetarian diets increase SHBG, which results in less free estradiol and testosterone. The most frequent causes of increased SHBG are aging and excess estrogen. SHBG is decreased by elevated or oral androgens, hypothyroidism, excessive glucocorticoids (steroids), obesity, excess insulin, progestins, growth hormone, and a low fat high fiber diet, resulting in more free estradiol and testosterone. The most frequent causes of low SHBG are insulin resistance and hypothyroid. These issues must be addressed to determine the cause of low or high testosterone levels.
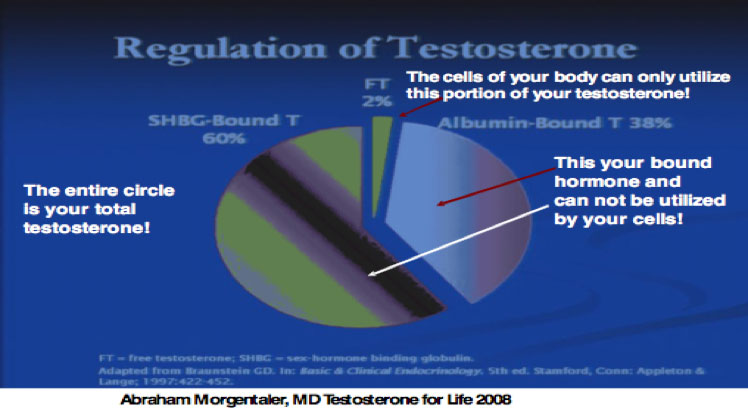
Figure 3 demonstrates the effect of aging on free testosterone.

In the graph in the left upper corner, the total testosterone shows minimal changes. But in the right upper portion of the graph, the free testosterone declines significantly because of the increase in the SHBG in the lower right portion.
Low Testosterone Signs and Symptoms
The signs and symptoms of low testosterone include [1]:
- Incomplete sexual development, aspermia (lack of sperm)
- Reduced sexual desire (libido) and activity
- Decreased spontaneous erections
- Breast discomfort, gynecomastia
- Loss of body hair (axillary, pubic)
- Decreased frequency of shaving
- Very small or shrinking testes (< 5 ml)
- Inability to conceive, low or zero sperm counts
- Height loss, low bone mineral density, low impact traumatic (pathologic) fracture
- Hot flushes, sweating, mood irritability
- Decreased energy, motivation, initiative, aggressiveness, self‐confidence
- Depressed feelings, dysthymia
- Poor concentration and memory
- Sleep disturbance, increased sleepiness
- Mild normochromic anemia (HCT 35‐39%)
- Increased body fat, BMI
- Diminished physical or work performance
Psychological Symptoms
The psychological symptoms of low testosterone include:
- Mood changes
- Poor concentration
- Loss of motivation
- Reduced initiative
- Memory impairment
- Anxiety
- Depression
- Irritability
- Insomnia
- General reduction in intellectual activity
Screening Questionnaire
One of the tools used to diagnose low testosterone is the ADAM Questionnaire [2].
- Do you have a decrease in libido?
- Do you have a lack of energy?
- Do you have a decrease in strength and/or endurance?
- Have you lost height?
- Have you decreased an “enjoyment of life”?
- Are you sad and/or grumpy?
- Are your erections less strong?
- Have you noted a decrease in ability to play sports?
- Are you falling asleep after dinner?
- Has there been a recent deterioration in work performance?
Positive screen = YES for # 1‐7 or any 3 questions
Testosterone Stimuli
The stimulus to produce testosterone begins in the hypothalamus as shown in Figure 4.
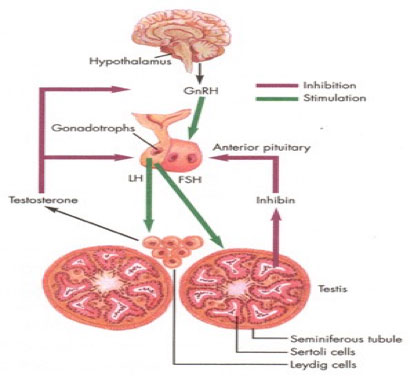
GnRH is gonadotropin-releasing hormone. LH is the pituitary hormone, luteinizing hormone and FSH is follicle-stimulating hormone. LH stimulates the testicle to make testosterone and FSH stimulates sperm production.
If a man less than 60 years old presents with low free testosterone, the question is, “Why is it low?” Is a problem in the hypothalamus, the pituitary gland or the testicles? The decision to place him on testosterone replacement therapy without an appropriate evaluation is inappropriate. If the LH is less than 5, this may indicate a problem in the hypothalamus.
Many factors affect the production of GnRH, including norepinephrine, dopamine, excess leptin (Leptin Control, ResveraTri), insulin resistance (Berberine, ALAmed CR, ALAmax Protect), lack of nitric oxide (Nitric Balance, N.O. Max ER) and excess cortisol (Adrenadapt) just to name a few. Again, you must consider all the factors previously mentioned. GnRH may be stimulated by a medication called Clomid, the protocol for which is listed below.
Clomiphene Stimulation
Used to test for hypothalamic / pituitary unit functioning in younger individuals (<60-65 years old)
Clomiphene 25 mg (50 mg tablet -1/2 tablet) hs for 7 days
Check pre and post FSH / LH, Testosterone, total, E2
Responses: Increased FSH/LH to >50% above baseline (hypothalamus/ pituitary unit intact)
Significant increase in testosterone> 50% (testes OK)
If robust response > 700 ng/dl, low dose clomiphene
10 – 25 mg three times weekly may be used to increase testosterone production
If the response is positive, LH and testosterone will double, and the man takes 25 mg of Clomid three times a week while the cause of the low GnRH is determined and treated appropriately. Once that problem has been resolved, the Clomid may be discontinued.
If the patient fails to respond to Clomid, that may mean the problem is in the pituitary gland. Human chorionic gonadotropin (HCG) is a similar molecular structure as LH. The HCG protocol is listed below.
Chorionic Gonadotrophin Stimulation Test
Chorionic Gonadotrophin (CG) 10,000 units per vial – reconstitute with 5 cc – 0.5cc = 1000 units
Train patient to self-administer in anterior thigh using saline in 50 unit insulin syringe with 30 Gauge 5/16” needle (painless)
Give CG 500 units (0.25cc) nightly, Sun – Tue – Thur for 2 weeks
Obtain blood test for testosterone, total and free and E2 on the second Friday a.m.
Continue CG Mon., Wed., Fri. until results are available (usually 1 week)
If the man fails to respond to the HCG, the dysfunction is probably in the testicle.
Why go to all this trouble? Why not just place him on testosterone replacement therapy and avoid the above protocols. The question is, ”Why is testosterone low?” Normal testosterone is pulsatile, meaning it spikes throughout the day. There is no form of testosterone replacement therapy that can match the pulsatile production of testosterone that produces the maximum benefit to a man’s health.
Some of the other causes of low testosterone are illustrated in Figure 5.
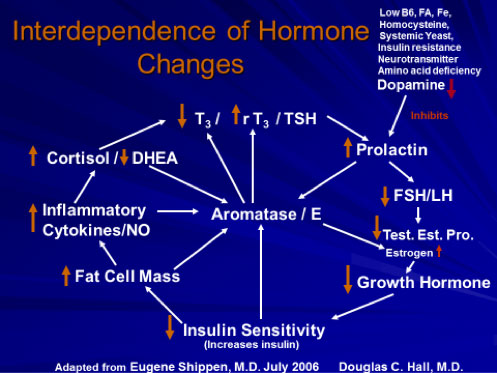
Failure to evaluate all of the above factors and merely place men on testosterone may lead to serious health consequences in the future. Each of these factors is discussed on this website.
The Power of Nutrition
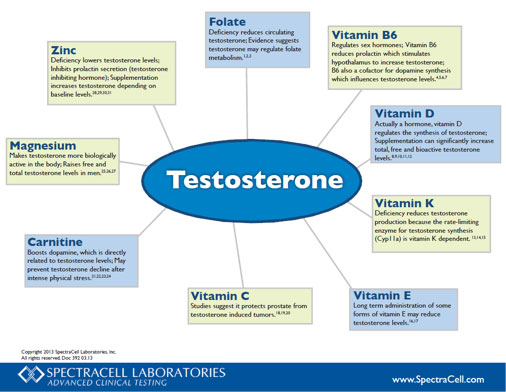
Nutrition plays a major role in all the reactions noted above. For example, low B6, iron and activated folate (5-MTHF) are involved in many of the pathways shown in Figure 5. A complete micronutrient through SpectraCell Laboratory is quintessential in determining the etiology of low testosterone. Look at Figure 6.
Other important Vitamins are magnesium (MAGnificent, Optimag), Zinc Glycinate, D3 Active 5000, K2-45, carnitine (Carnite MD), vitamin C (Bioflav-C, xcellent C), and vitamin E (E-ssential).
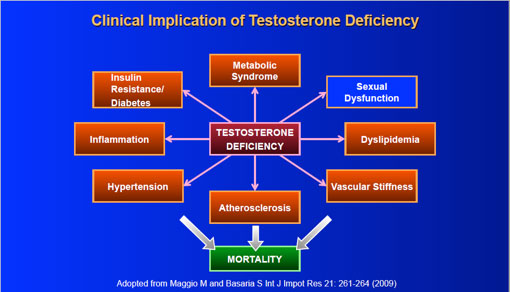
Low Testosterone and Overall Health
Why is all this so important? Low testosterone has been associated with an increased risk of adverse medical conditions, including an increased risk of
Type 2 diabetes, metabolic syndrome, stroke, dementia, heart disease, frailty syndrome, inflammation and cancer.
Men with low testosterone also tend to have these heart disease risk factors:
- Atherosclerosis
- Angina pectoris
- Insulin resistance/diabetes
- High blood glucose
- High LDL cholesterol
- High triglycerides
- High blood pressure
- High body mass index (obesity)
- High hip-to-waist ration
- High levels of blood clotting factors
A study published in JAMA 2005;294(23):2996‐3002 revealed that men with ED and no history of a previous cardiovascular event have a 15% chance of a cardiovascular event in 7 years.
The symptoms of low testosterone include:
- Diminished libido
- Erectile dysfunction
- Difficulty achieving an orgasm
- Decreased spontaneous erections
- Diminished energy, sense of vitality or well-being
- Fatigue
- Depressed mood
- Impaired cognition
- Reduced motivation
- Breast enlargement
- Increased body fat
- Decreased muscle mass and strength
Look at Figure 7.
The Issue of Age
It is well established that testosterone decreases with age. How common is hypogonadism in older men?
Prevalence of Hypogonadism When Measuring Total Testosterone3:
<5% for men in 20s & 30s
12% for men in 50s
19% for men in their 60s
28% for men in their 70s
49% for men >80
Aging is associated with declines in total serum testosterone concentration, increases in SHBG concentration, and decreases in free testosterone. In one large cross-sectional study of more than 3,000 men ages 40 to 79, serum testosterone concentration fell 0.4% per year and free testosterone concentration fell 1.3%4. In another study of 890 men, total testosterone levels were <325 ng/dL (considered androgen deficient) in 20%, 30%, and 50% of men in their 60s, 70s, and 80s, respectively. [5]
Epidemiologic studies have repeatedly found associations between low serum testosterone in men and the subsequent development of central obesity, higher insulin concentrations, metabolic syndrome, and diabetes. [6]
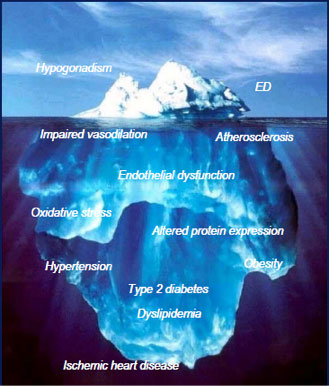
ED and Hypogonadism
As you can see in Figure 8, hypogonadism is really just the tip of the iceberg when it comes to ED (erectile dysfunction).
Medical Conditions and Low Testosterone
The following conditions are associated with low testosterone [7]:
- T2DM / morbid obesity / metabolic syndrome (treatment with acute or chronic medications that affect T production and/or metabolism)
- Glucocorticoids
- Anti‐fungal medications
- Opioids
- Spironolactone (diuretic)
- 5‐alpha reductase inhibitors (decrease conversion of testosterone to DHT (dihydrotestosterone)
- HIV‐associated weight loss
- End‐stage renal disease and hemodialysis
- Moderate to severe COPD
- Infertility
- Osteoporosis or low‐trauma fracture, especially in young men
- Sellar mass, radiation to sellar region
The Easy Solution – Testosterone Replacement Therapy
There are numerous studies demonstrating the benefits of testosterone replacement therapy in improving the quality and length of life.
In J Clin Endocrinol Metab 2012;97(6):2050‐2058, 1,031 men 40 years of age or older with low testosterone were followed for 48 months. The men who were treated with testosterone had a mortality risk of 10.3% whereas the untreated men’s mortality risk was 20.7%.
Testosterone replacement therapy does not cause prostate cancer. The study indicating there was a relationship between testosterone and prostate cancer was published in 1941 and based on one patient. In fact, high-grade aggressive prostate cancer is associated with low serum testosterone levels.
There is still some disagreement in the literature concerning what level of serum testosterone should be used to diagnose hypogonadism and its subsequent treatment. While the Food and Drug Administration uses a cutoff of 300 ng/dL to define hypogonadism for clinical trials, a consensus statement from several professional societies recommends no treatment for patients with T levels above 350 ng/dL; treatment for levels below 230 ng/dL in symptomatic patients; and repeat testing for patients with levels between 230 and 350 ng/dL. [8]
Treatment should be individualized based on laboratory and symptoms, not just data only.
The Goal of Therapy
Take a look at Figure 9.
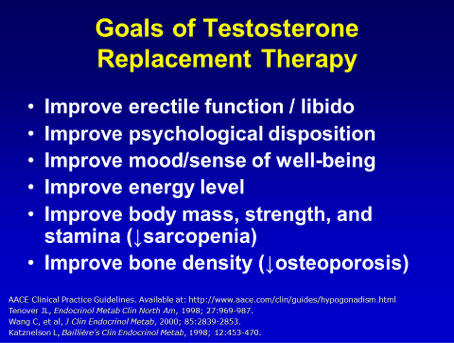
Testosterone supplementation can help reduce many of the symptoms associated with androgen deficiency in aging males by its effects on various parts of the body. Bone mineral density can decrease in the hypogonadal men and this may contribute to the increased fracture rate in the elderly. Testosterone therapy can improve bone mineral density and bone architecture by increasing bone formation and decreasing bone resorption, but the possible benefits on fracture rate are unknown. Testosterone also improves body composition by reducing body fat mass and increasing lean body mass, and increasing epidermal thickness, but its effects on muscle strength are still debated.
In patients with diabetes and androgen deficiency, testosterone supplementation appears to reduce blood glucose and this could have important implications for cardiovascular risk reduction in patients with diabetes or the metabolic syndrome. The wide-ranging benefits of testosterone therapy in young and old men are clear and it appears that the route of administration (intramuscular, oral, or transdermal) does not alter this fact, but future work could illustrate even more profound effects of testosterone (e.g., in reducing cardiovascular risk) that could result in its recommended use in a wider range of patients. [9]
Is it safe?
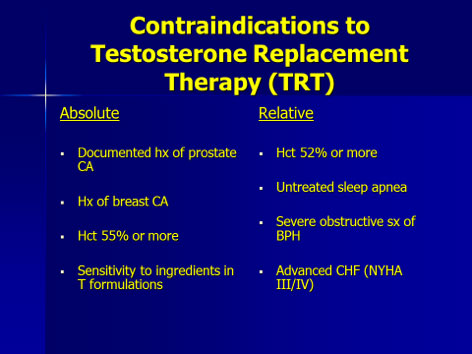
Figure 10 shows the absolute and relative contraindications to testosterone replacement therapy.
In 2013 and 2014, two articles appeared in the literature indicated that testosterone therapy increased the risk of heart attack and stroke. The title of those articles appears in Figure 11.
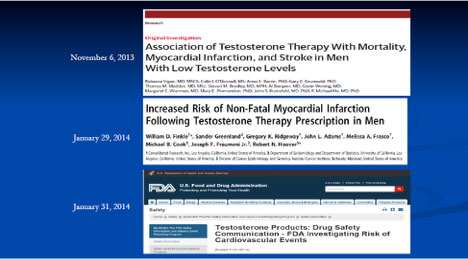
Naturally, this made headline news and attorneys were celebrating. Take a look at Figure 12.

What Experts are Saying
However, numerous experts across the world evaluated these studies and found them to have numerous design flaws, meaning the data was not valid. They asked the editors of these journals to have the invalid studies retracted from the literature. To resolve this problem, experts met on October 1, 2015 in Prague, Czech Republic to find common ground: “What is true that we can agree on?” A urology specialist from the U.S., Abraham Morgentaler, served as chair, and 18 experts in testosterone metabolism attended from 11 countries and 4 continents.
After hearing from all the experts, they decided on nine resolutions:
- Testosterone deficiency is a well-established, significant medical condition that negatively affects male sexuality, reproduction, general health, and quality of life. Testosterone deficiency:
- May predict increased risk of developing diabetes, metabolic syndrome
- Contributes to decreased bone mineral density
- Is associated with increased all-cause and cardiovascular mortality
- Negatively impacts general health and quality of life
- The symptoms and signs of TD occur as a result of low levels of testosterone, and may benefit from treatment regardless of whether there is an identified underlying etiology.
- Symptoms and signs of TD occur in healthy volunteers or patients who undergo androgen deprivation therapy; they resolve with T normalization.
- Historically recognized causes of TD are rare (e.g., anorchia, pituitary tumor), recently termed “classical hypogonadism.” TD occurs frequently with conditions other than “classical” causes. No evidence supports restriction of T therapy only to men with known underlying etiology.
- Newly Recognized Causes of T Deficiency:
- Diabetes
- Obesity
- HIV/AIDS
- Glucocorticoids
- Opioids
- Aging
- Testosterone deficiency is a global health concern. Prevalence rates in adult men range from 2% to 38% in studies from Asia, Europe, North America and South America. Variation in prevalence rates is explained by differences in operative definition of TD and biochemical thresholds. A U.S. study estimates an additional $190-525 billion in healthcare expenditures over 20 years due to TD.
- Testosterone therapy for men with TD is effective, rational and evidence-based. High-level evidence shows T therapy effectively:
- Increases sexual desire (libido) and erectile and orgasmic function
- Increases lean body mass
- Decreases fat mass
- Improves bone mineral density
- Improves mood and energy (strongly suggestive evidence exists)
- There is no T concentration threshold that reliably distinguishes those who will respond to treatment from those who will not. No study has revealed a single testosterone threshold that reliably separates those who experience signs and symptoms of TD from those who do not, or who will likely to respond to treatment.
- Interpretation of total T concentrations confounded by:
- Inter-individual variation
- Variation in serum SHBG (binds tightly to T, theoretically removing it from the bioavailable pool)
- Genetic variation in androgen sensitivity due to ARd gene polymorphisms (number of CAG repeats)
- Free testosterone can be useful indicator of androgen status.
- There is no scientific basis for any age-specific recommendations against the use of T therapy in adult men. “Age-related hypogonadism” is of questionable validity, since the decline in mean serum T with age is minor and attributable to comorbidities, especially obesity. Older men respond well to T therapy, as do younger men.
- The increased risk of erythrocytosis in older men requires monitoring, but does not merit withholding T therapy if indicated. It is illogical to single out TD as the one medical condition among many (e.g., diabetes, hypertension, heart disease, cancer, arthritis) that does not merit treatment because it becomes more prevalent with age.
- The evidence does not support increased risks of cardiovascular events with T therapy. The media focused on two observational studies that reported increased CV risks, but both had major flaws/limitations.
- Low serum T is associated with increased atherosclerosis, coronary artery disease, obesity, diabetes and mortality. Several RCTs in men with known heart disease (angina, heart failure) showed greater benefits with T versus placebo (greater time to ischemia, greater exercise capacity). The largest meta-analysis showed no increased risk with T therapy; a reduced risk was noted in men. There was also no increased risk of veno-thrombotic events with T therapy.
- The evidence does not support increased risk of prostate cancer with T therapy.
- Serum androgen concentrations are not associated with increased risk of PCa or aggressive disease. T therapy shows no greater risk of PCa than placebo.
- Aggressive/high-grade PCa is associated with low serum T levels.
- Early data suggests no increased risk of recurrence/progression with T therapy in men previously treated for PCa. A large body of evidence suggests lower serum T concentrations are associated with increased CV risk; higher levels are protective T therapy, reliably increasing lean mass, decreasing fat mass, and possibly improving glycemic control
- Mortality rates reduced by half in men with TD who receive therapy compared with untreated men in observational studies. Among men who received T therapy, those with normalized T had reduced rate CV /mortality versus men with persistently low T.
In summary, there is no convincing evidence of increased CV risks with T therapy. On the contrary, there appears to be a strong beneficial relationship between normal T and CV health that has not yet been widely appreciated..”
The conclusion is clear: testosterone therapy is safe, but it must to be monitored properly to ensure safety. Take a look at Figure 13.
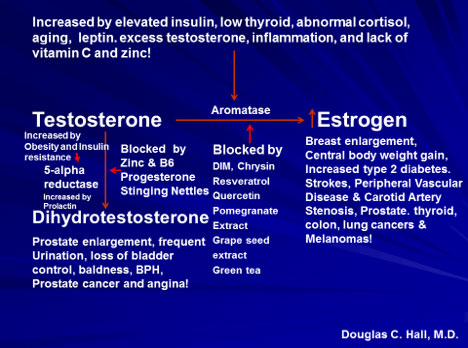
A baseline value of total and free testosterone, estradiol, SHBG, and dihydrotestosterone (DHT), along with other lab data, must be obtained prior to initiating therapy. The aromatase enzyme converts testosterone to estrogen (estradiol). The factors that increase the activity of aromatase are listed at the top of the diagram. In the middle of the graph are listed the many substances that inhibit aromatase. The potential consequences of excess estrogen are listed in the right-hand column, while the left side of the diagram shows the enzyme that converts to DHT is 5-alpha reductase. This enzyme activity is increased by excess testosterone, obesity, insulin resistance and elevated prolactin. The potential consequence of excess DHT, are listed above. The enzyme may be inhibited by progesterone (ProgX), B6, zinc and stinging nettle, just to name a few.
The importance of normal estradiol level is reflected in Figure 14.
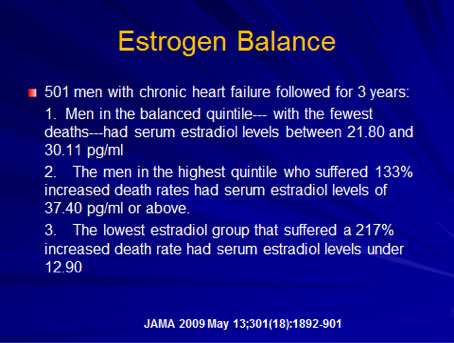
To start an individual on testosterone therapy and not monitor the above values may lead to serious adverse health consequences.
Potential Consequences of Testosterone Replacement Therapy
Some of the potential consequences of testosterone replacement therapy are:
- Erythrocytosis (increase red blood cells and most common in IM and subcutaneous preparation and dose related. Theoretic risk of thrombotic event [blood clot], but no reported cases. Treated by dose reduction, blood donation or therapeutic phlebotomy.) Worsening of sleep apnea
- Infertility
- Gynecomastia (breast enlargement)
- Fluid retention in the extremities
- Decrease in testicular size
- Skin reactions
- Acne/oily skin
- Increased body hair
When Therapy is Not Recommended
Therapy is not recommended for men who have [10]:
- Prostate or breast cancer
- A nodule on the prostate that can be felt during a DRE
- A PSA greater than 3 ng/ml without further evaluation
- A hematocrit greater than 50% or thick, viscous blood
- Untreated obstructive sleep apnea
- Severe lower urinary tract symptoms
- Class III or IV heart failure
Forms of Therapy
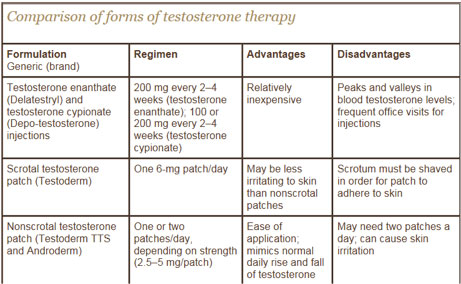
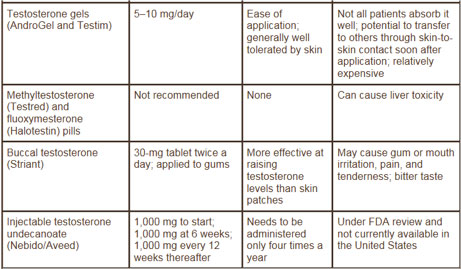
The advantages and disadvantages of the various forms of therapy are listed in Figure 15.
Want to learn more about testosterone replacement therapy from an expert? Visit http://www.harvardprostateknowledge.org/a-harvard-expert-shares-his-thoughts-on-testosterone-replacement-therapy.
Testosterone Pellets
The most effective therapy is testosterone pellets. They have been used since 1940. Pellets are implanted in the subcutaneous tissue of the lower abdominal wall or buttocks in a minor surgical procedure that takes about 10 minutes. Three to six 200 mg pellets provide a physiological dose of testosterone for 4-6 months. It is an effective dose of therapy with complete bioavailability. There is no elevation of estradiol or DHT. There is a transient accelerated release rate for 1-2 days only, an extrusion rate of 5%, minor bleeding 2%, and infection rate of <1%.
Pellets deliver consistent, physiological levels of testosterone. Pellets avoid the fluctuation of hormone level that’s seen with every other method of delivery. It is the fluctuation in testosterone level that cause many symptoms. Pellets do not increase the risk of blood clots like the conventional oral or synthetic HRT. Pellets are superior to oral, conventional hormone replacement therapy, especially with respect to bone density, insomnia, sex drive, libido and sexual performance. Pellets are the most convenient method of hormone delivery.
Studies have shown that patients treated with pellet implants have:
- Increased energy
- Improved sleep
- Relief of depression and decreased anxiety
- Increased muscle mass and bone density
- Decreased soft fatty tissue
- Increased coordination and physical performance
- Improved skin (increased collagen and elastin)
- Increased concentration and memory
- Improved overall physical health (BP, lipids, glucose)
- Improved libido and sexual satisfaction
- No increased risk of blood clots
References
- Bhasin S, et al. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society Practice Guideline. J Clin Endocrinol Metab 2010;95(6):2536-2559.
- Androgen Deficiency in Aging Males. Morley JE, Charlton E, Patrick P, et al. Metabolism 2000;49(9):1239-1242
- Harman SM, Metter EJ, Tobin JD, Pearson J, Blackman MR. Longitudinal effects of ageing on serum total and free testosterone levels in healthy men. Baltimore Longitudinal Study of Aging. J Clin Endocrinol Metab 2001; 86(2): 724-31.
- J Clin Endocrinol Metab. 2008;93:2737-2745
- J Clin Endocrinol Metab. 2001;86:724-731
- Diabetes Care. 2004;27:1036-1041, Diabetes Care. 2002;25:55-60
- Bhasin S, et al. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society Practice Guideline. J Clin Endocrinol Metab 2010;95(6):2536-2559.
- Urology. 214:83;980-988
- Aging Male. 2006 Dec;9(4):183-8
- Endocrine Society
Supports healthy testosterone levels, healthy libido and performance, and overall vitality; optimizes physical strength and endurance; and supports sense of healthy mental and physical well-being.
Supplementation with magnesium increases free and total testosterone values in sedentary individuals and athletes. The increases are higher in those who exercise than those who have a sedentary lifestyle.
Several active leads exist regarding the role of micronutrients and metabolites in prostate cancer carcinogenesis and risk. How vitamins D and A may adversely impact risk, and whether low-dose vitamin E supplementation remains a viable preventive approach, require further study.
Supports detoxification of xenoestrogens.
Secondary and compensated hypogonadism are associated with vitamin D deficiency.
Methylation is essential for the proper metabolism of testosterone.
Zinc inhibits 5 alpha reductase, which converts testosterone to dihydrotestosterone.
A higher consumption of green tea is associated with a lower prevalence of cognitive impairment. Low testosterone leads to poor cognitive function.
Osteo MK-7 uses an array of complementary, well-researched nutrients to build and maintain bone, especially during andropause (low free testosterone).
Improves the metabolism of testosterone in Phase I and II detoxification.
Omega-3 fatty acids have been used in the treatment and prevention of Alzheimer’s disease, prostate and colon cancer, depression, anxiety, heart disease, hypertension, high cholesterol, obesity, osteoporosis, skin disorders, and strokes.
Supports healthy testosterone metabolism.

About the Author
Douglas C. Hall, M.D.
Dr. Douglas Hall, was born in Indianapolis, Indiana on Jan. 30, 1941. He received his BS and Doctor of Medicine at the University of Florida, training in obstetrics and gynecology. Dr. Hall has been in private practice since 1974 and currently has a large practice in Ocala, specializing in OB/GYN and Functional Medicine.

