Learn About the Prostate Gland and its Functions
Function of the Prostate
What causes BPH?
The Role of Excess Estrogen
The Thyroid Affect
The Role of Cortisol
Balancing the Estrogen in Men
Blocking the Conversion of Testosterone to DHT
Focusing on Nutrients
Evaluating BPH and Potential Causes
Other Treatments
The Function of the Prostate
The prostate is part of the male reproductive system. It’s about the size of a walnut and weighs about an ounce. The prostate is below the bladder and in front of the rectum. It goes all the way around a tube called the urethra, which carries urine from the bladder out through the penis. Its function is to store and secrete a clear, slightly alkaline fluid that constitutes 10-30 % of the volume of seminal fluid, which along with the spermatozoa, constitutes semen.
The high prevalence of BPH can be appreciated when it’s compared with other common conditions. Its prevalence in men older than 60 is greater than the prevalence of diabetes in adults over 65 years and asthma in the population at large. Approximately half of men in the sixth decade of life exhibit histologic evidence of BPH, and almost 90% develop histologic BPH by the ninth decade of life. (Rev Urol. 2004; 6(Suppl 9): S3–S10.)
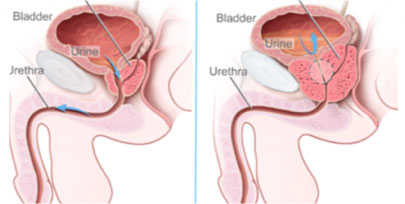
As depicted in Figure 1, on the left is a normal prostate surrounding the urethra. On the right is an enlarged prostate compressing the urethra, partially compressing the base of the bladder, and applying pressure against the rectal area posteriorly. BPH is a very complex disease with multiple causes. It’s increasing in frequency because of the aging population.
The various symptoms of BPH, referred to as lower urinary tract symptoms (LUTS), include:
- Frequent urination, especially at night
- Feeling that the bladder is full, even right after urinating
- Feeling that urinating “can’t wait”
- Weak urine flow
- Dribbling of urine
- The need to stop and start urinating several times
- Trouble starting to urinate
- The need to push or strain to urinate
In severe cases, the urethra becomes completely compressed and urination is impossible. This is referred to as bladder outlet obstruction (BOO), and requires immediate attention. These symptoms are frequently associated with erectile dysfunction and can negatively affect a man’s quality of life. Once of the best solutions to this problem is found in Curcuminoid CR. This will help reduce inflammation and provide relief. There is a great tool to help men determine the severity of their BPH. You can find more information here. It is a questionnaire called the International Prostate Symptom Score (I-PSS).
What causes BPH?
As mentioned earlier, the true cause has not been determined, but many factors contribute to the development of BPH, including lack of sunlight, smoking, pesticide exposure, rotating shift work, lack of physical activity, aging, family history of BPH, obesity, erectile dysfunction, excess estrogen, and a hormone called dihydrotestoterone (DHT).
Dietary risk factors include total fat intake, animal fat intake, and red meat consumption; cooking red meat at high temperature or on a grill; and excess consumption of commercial dairy products.
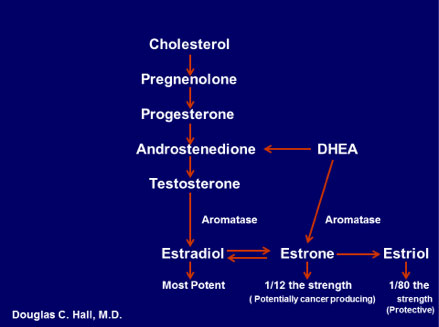
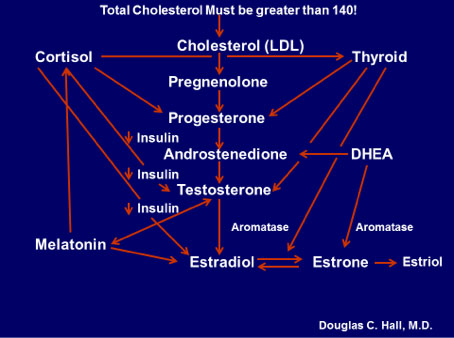
As we have discussed hormones play a big part on how hormones affect BPH is affected starting with estrogen. Figure 2 below notes that the production of hormones begins with cholesterol and is affected by DHEA, which is produced by the adrenal glands on top of the kidneys. These hormones do not work in isolation.
The Role of Excess Estrogen
It’s established that men need estrogen, but not in excess, since that’s been associated with BPH, prostate cancer and other metabolic disorders. The next obvious question is, “How does a man produce too much estrogen?” DIM-3 is a great way to help lower estrogen levels.
Look at the arrow that goes from testosterone to estradiol, which is the most potent estrogen. That enzyme, called aromatase, converts testosterone to estrogen when activity is increased due to excess insulin, low thyroid, abnormal cortisol, inflammation, lack of vitamin C and zinc, just to name a few. Zinc Glycinate is a quick way to help restore overall health. The highest concentration of zinc in the entire body is in the prostate gland.
Figure 4 below depicts how the fatty tissue in the breast and abdomen produces inflammation, which increases the aromatase enzyme and converts testosterone to estradiol.
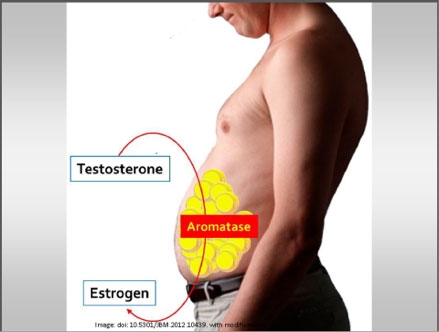
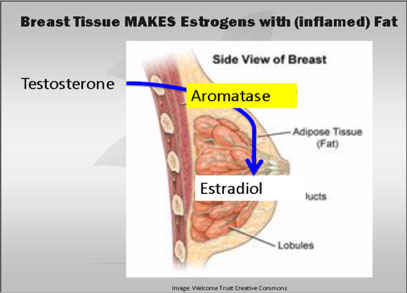
Figure 4
Endocrine Disruptors
There are certain chemicals we are exposed to on a daily basis that alter how hormones are produced and metabolized. These are called endocrine disruptors. There is no end to the tricks that endocrine disruptors can play on our bodies: increasing production of certain hormones while decreasing production of others, imitating hormones, turning one hormone into another, interfering with hormone signaling, telling cells to die prematurely, competing with essential nutrients, binding to essential hormones, and accumulating in organs that produce hormones. The most common ones are BPA, Dioxin, Atrazine, Phthalates, Perchlorate, fire retardants, lead, arsenic, mercury, perfluorinated chemicals (PFCs), organophosphate pesticides, and glycol ethers! Please learn about the Dirty Dozen Endocrine Disruptors.
The Thyroid Affect
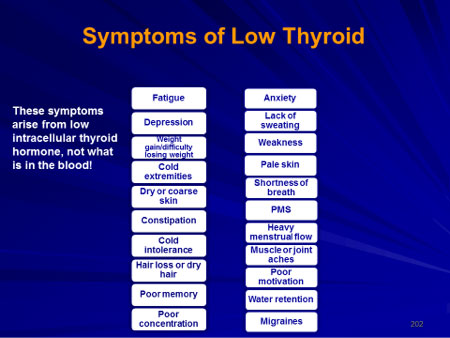
Now let’s turn our attention to the thyroid and how it can affect estrogen levels. Once a hormone has performed its function, it must be detoxified through the liver. This requires multiple metabolic pathways and adequate amounts of macro and micronutrients. The thyroid hormone plays a major role in phase 2 detoxification. If you have inadequate macro or micronutrients, you’ll have impaired detoxification, which will allow estrogen to bio-accumulate in the tissues, including the prostate gland. The same principle applies for inadequate thyroid hormones. Remember low thyroid is a clinical diagnosis and not based on laboratory results. Look at Figure 5.
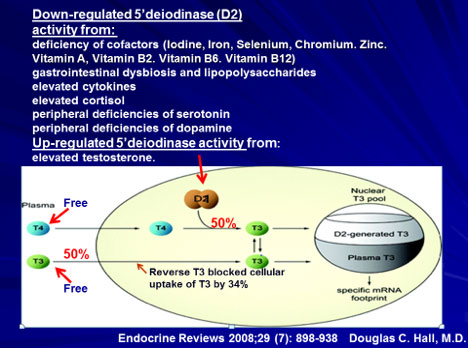
The thyroid gland produces mainly T4 and small amounts of T3. However, the active hormone is T3. The conversion of T4 to T3 occurs in the liver and the peripheral tissues. In Figure 5, you’ll see T4 and T3 in the blood vessel to the left. Since T3 activates the gene, it goes right to it for activation. However, T4 is transported into the cell and must be converted there to T3 to activate the gene.
No one can measure how effective T4 is converted to T3 to activate the gene to carry out the normal function of the cell. But someone who has poor conversion within his cells can certainly feel its effect. A blood test is a guess! It’s more important to ask the person how he feels. I’ve listed in upper portion of the diagram some of the many factors that block the conversion within cells. See the thyroid section for the many factors that inhibit the conversion of the inactive hormone T4 to the active hormone T3. If a man has several of the symptoms noted in Figure 6, he more than likely has low thyroid function (hypothyroid), which may play a role in BPH because of a failure to metabolize estrogen properly.
The Role of Cortisol
Now let’s take a look at how abnormal cortisol could play a role in BPH. The adrenal glands sit on top of the kidneys and are about the shape of walnut. One of the hormones produced by the adrenal glands is cortisol, in response to three major conditions: abnormal glucose metabolism, stress and inflammation. Figure 7 lists the various functions of cortisol.
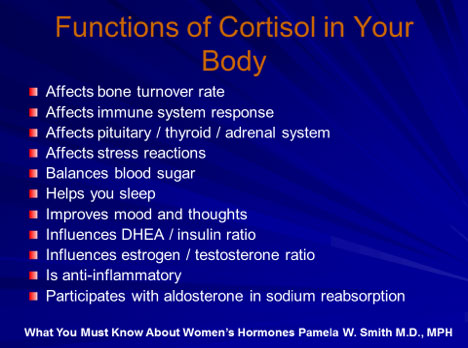
Cortisol affects thyroid, blood sugar, sleep, DHEA/insulin ratio, and estrogen/testosterone ratio, and is anti-inflammatory. All those factors can directly or indirectly affect estrogen metabolism and increase the risk of BPH.
Melatonin has a direct effect on testosterone and estrogen as depicted earlier in Figure 3. Since serotonin produces melatonin, neurotransmitters must also be evaluated, including serotonin, GABA, dopamine, norepinephrine, epinephrine and glutamate. Adequate levels of serotonin and dopamine are required to convert T4 to T3, and adequate serotonin is required to stimulate TRH, which stimulates TSH for normal thyroid function.
Balancing the Estrogen in Men
The microbiome must also be considered as a source of estrogen. A great solution for this is ResveraTri. When 100 trillion cells in the microbiome are in balance, it provides men with numerous benefits. It actives AMPK, conserves ATP and simultaneously enhances generation of ATP, enhances glucose uptake, enhances lipolysis, enhances protein synthesis, enhances glycogen synthesis, enhances mitochondrial biogenesis, decreases ROS/oxidative stress, and has a major effect on the immune function. An abnormal microbiome may increase an enzyme called glucuronidase, which will break the bond between estrogen and glucuronide and recycle the estrogen back into the body. It essential that this enzyme be evaluated in a stool test in anyone who has BPH or any estrogen-related cancer. Other factors, some of which have been mentioned earlier, increase estrogen levels in men, according to Pamela W. Smith, M.D., MPH:
- Obesity
- Zinc deficiency
- Grapefruit
- Alcohol abuse
- High doses of Vitamin E
- Environmental estrogens
- Aromatization of hormones
- Pain relievers: acetaminophen, NSAID, ASA, propoxephene
- Antibiotics: sulfas, tetracyclines, penicillins, cefazolins, erthyromycins, quinolones
- Antifungal agents
- Antidepressants: fluoxetine, fluvoxamine, paroxetine, sertraline
- Anti-psychotic medicines: thorazine, haloperidol
- Antacids: omeprazole, cimetidine
- Abuse substances: alcohol, amphetamines, marijuana, cocaine
- Heart and blood pressure medicines: propranolol, quinidine, amiodarone,
- Coumadin, methyldopa
- Cholesterol-lowering drugs
However, there are some substances and drugs that lower estrogen levels, including:
- Vitamins: high doses of Vitamin C, Vitamin K, niacin
- Foods: soy, vegetarian diets, cruciferous vegetables, oysters, resveratrol (grape skin compound)
- Chrysin
- Arimidex
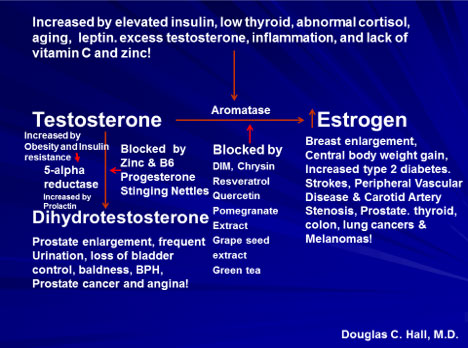
As previously noted, the conversion of testosterone to estrogen involves the aromatase enzyme. Figure 8 notes the factors that increase aromatase activity and convert more testosterone to estrogen, which increases prostate size, and the factors that inhibit aromatase, therefore decreasing estrogen and prostate size. Arimidex is prescription medication that is an aromatase inhibitor. The dose is .5 mg Monday and Thursday only. By controlling the factors that stimulate aromatase and consuming dietary supplements that inhibit aromatase, the conversion of testosterone to estrogen can be limited, which reduces prostate size and the symptoms of BPH.
Another Theory
Another theory of the cause of BPH focuses on dihydrotestosterone (DHT), a male hormone that plays a role in prostate development and growth. Some research has indicated that even with a drop in blood testosterone levels, older men continue to produce and accumulate high levels of DHT in the prostate, which may encourage prostate cells to continue to grow. Scientists have noted that men who do not produce DHT do not develop BPH.
As noted in Figure 8, testosterone is converted to DHT by the enzyme called 5-apha reductase, which has two types: type 1 and type 2. Type 1 is the predominant enzyme in extraprostatic tissues, such as skin and liver. Type 2 is the predominant enzyme in prostatic tissue, although it’s also expressed in extraprostatic tissue (sebaceous glands and acne). Obesity and insulin resistance activate the enzyme, the same factors that increase the aromatase enzyme that converts testosterone to estrogen. It is also increased by prolactin, which increases with age, but is decreased by adequate levels of zinc and progesterone (ProgX). Increased DHT will increase prostate size and symptoms of BPH. DHT has a growth-promoting effect on prostate cells that is greater than that of testosterone by 2.4-10 times. (Mol Cell Endocrinol 1992; 88(1-3):15-22)
Blocking the Conversion of Testosterone to DHT
Medications that block the conversion of testosterone to DHT are called 5-alpha inhibitors. See Figure 9.
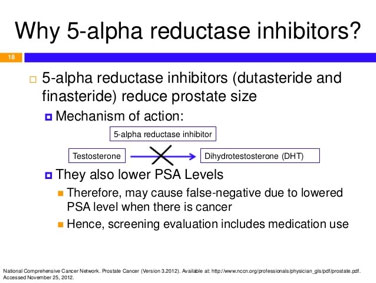
The three most popular 5-alpha inhibitors are Propecia, Finasteride (Proscar) and Dutasteride (Avodart). Propecia only inhibits type 2 5-alpa reductase, Proscar inhibits type 2 5-alpha reductase, and Avodart inhibits both types. All three are less effective in relieving BPH symptoms than the alpha-1 blockers.
Avodart is 2.5 times more potent in inhibiting type 2 (the main enzyme in prostate tissue) than Proscar; it can reduce prostate size by 93%. Avodart’s side effects include decreased libido, impotence, decreased volume of ejaculate and decreased testosterone levels.
There are many natural 5-alpha reductase natural inhibitors, including Astaxanthin, Black Cohosh, Saw Palmetto, Willow Herb, Beta Sitosterol, Mangiferin, Reishi (Ganoderma), Cactus Flower, Pygeum Africanum, and an extract of the root of the stinging nettle plant (Urtica dioica).
Pollen extracts are very helpful in reducing the effects the symptoms of BPH by three different mechanisms. They inhibit 5-alpha reductase, are anti-inflammatory and are alpha-1 adrenergic receptor blockers. D3 Active 5000 is also a great solution in reducing the effects of BPH.
A reduction of approximately 50% in prostate-specific antigen (PSA) within 12 months is expected in men taking 5-alpha reductase inhibitors.
A small prostate with alpha-1 adrenergic receptors may still produce symptoms of BPH as illustrated in Figure 10.
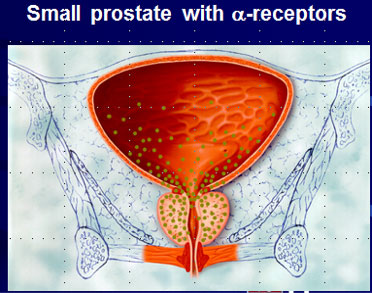
The dots in the prostate and bladder represent alpha-1 adrenoreceptors that maintain the tone of bladder and prostate tissue. When these receptors are stimulated by norepinephrine from adrenergic nerves, the tone of these tissues increases, further increasing the obstructive symptoms associated with BPH. The class of medications are used in the treatment of BPH to inhibit this reaction are listed in Figure 11.
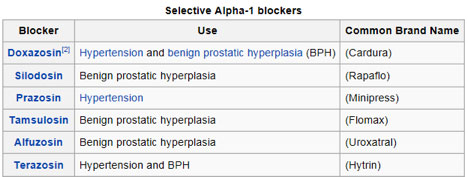
Tamsulosin (Flomax) is the most selective alpha-1 adrenergic blocker. Side effects of these medications include hypotension, dizziness, fatigue, ejaculatory disorder and nasal congestion.
Caffeine, alcohol, antihistamines and decongestants all tighten the bladder neck (activate the alpha receptor) and make it difficult to urinate.
PSA is now considered as an active growth factor in the prostate gland. It has an enzymatic ability to degrade extracellular matrix proteins such as fibronectin laminin, which may promote tumor growth. PSA also frees IGF-1 (see here and here) from its binding protein (BP-3), providing increased local levels IGF-1 that can lead to tumor growth.
Men who control their weight, inflammation, insulin resistance, micronutrients, and hormone balance through lifestyle, proper nutrition, and nutritional supplementation, will produce less estrogen and DHT, decreasing their risk of BPH.
Focusing on Nutrients
The nutrients required for normal prostate function include:
- Vitamin A, C and D
- Thiamin, Riboflavin, Niacin
- Calcium
- Iron
- Zinc*
*The prostate needs 10 times more zinc than other organs, needs it to combined with Vitamin B6 for better absorption, and needs it to be kept in proper ratio with copper [10:1]. Zinc absorption goes down with age.)
The nutrients that decrease the risk of prostate cancer include:
Evaluating BPH and Potential Causes
The following information is required to properly evaluate men for BPH:
- Complete Medical History and Physical with DRE
- Family History
- Medication and Supplement History
- Exercise History
- Dietary History
- Social History
- CBC, CMP, TSH, free T3, Free T4, reverse T3, TPO and Thyroglobulin antibodies, ferritin, fasting glucose and insulin, Hgb A1C, homocysteine, prolactin, cystatin C, total and free testosterone, SHBG, estradiol, DHT, total and free PSA, LH, FSH, IGF-1, IGF-1 BP-3, 4 point salivary cortisol test, neurotransmitter test, stool analysis, advanced lipid testing with particle size and number, and micronutrient analysis.
Differential diagnoses (potential causes of BPH) include:
- Urethral Stricture
- Bladder Neck Contracture
- Bladder Stones
- Urinary Tract Infection
- Interstitial Cystitis
- Neurogenic Bladder
- Inflammatory Prostatitis
- Medications
- Carcinoma of the prostate
- Carcinoma in situ of the bladder
- Treating BPH
Treatment will depend on a unique evaluation, including the severity of the symptoms. All abnormal laboratory findings must be corrected in an attempt to maintain hormone balance to reduce the production of excess estrogen and DHT. The micronutrients must be returned to adequate levels to ensure proper metabolism and detoxification. All lifestyle factors and environmental factors that are contributing to the dysfunction must be addressed and corrected if possible. The goal is to address the cause(s) and not just treat the symptoms. The standard treatments are listed below:
- Medical
- Minimally invasive and endoscopic
- Surgical
The first line of defense against bothersome urinary symptoms:
- Alpha-1 blocker that relaxes the prostate and provides a larger urethral opening (Tamsulosin {Flomax}, Silodosin {Rapaflo})
- Shrink the prostate gland with a 5-alpha reductase inhibitor (Finasteride {Proscar}, Dutasteride {Avodart}).
A combination therapy, using both an alpha adrenergic receptor blocker and 5-alpha reductase inhibitor has proven to be the most effective approach.
In addition, the natural 5 alpha reductase inhibitors listed above are very effective if used in combination. The natural aromatase inhibitors are also very effective in decreasing estrogen production.
Other Treatments
- Needle ablation of prostate (TUNA)
- Heat treatment inducing necrosis of prostatic tissue, where the aim is to increase prostatic temperature to an excess of 60 degrees Centigrade, using low level radiofrequency (RF) energy to produce localized necrotic lesions in the hyperplastic tissue.
- Laser treatments — various types (most popular is the green light laser)
- Transurethral resection of prostate (TURP) — gold standard of care for BPH. Uses an electric “knife” to surgically cut and remove excess prostate tissue. Effective in relieving symptoms and restoring urine flow.
Alternative Therapies
- Saw Palmetto: 320 mg twice a day
- Pygeum (beta-sitosterol): 60 mg a day
- Stinging Nettles: 120 mg twice a day
These can be found in one of the following formulas:
- Prosta-DHT
- Ultra Natural Prostate
- Prosta-Go
Combination Products
- Pomegranate whole fruit powder (OrganiX Phytofood)
- Broccoli powder
- Turmeric powder
- Green tea extract
Other nutrients include amino acids: glycine, alanine, and glutamic acid, which have helped as noted below:
- 92% reduction in prostate size
- 96% decrease in nocturia
- 81% less urgency to urinate
- 73% urinated less frequently
- 71% had reduced discomfort
Nutrition
- Consume omega-3 fish, e.g. wild salmon, sardines
- Avoid tuna due to mercury content
- Avoid farm-raised fish due to PCB contamination, which has xenoestrogen effects
- Consume a lot of omega-3 eggs
- Eat organic fruits and vegetables
- Avoid GMO foods
- Eliminate processed and fast foods
- Drink water, green tea and pomegranate juice
Summary
Following all these suggestions can reduce the incidence of BPH and its associated symptoms. It’s not convenient or easy, but if it’s done properly, the result is improved quality of life.
A study demonstrated that BPH or prostate carcinoma may be associated with a reduction in the levels of tissue and plasma zinc, and an increase in urine zinc/creatinine.
Helps lower excess estrogen levels and support healthy testosterone metabolism.
Supports healthy testosterone metabolism.
Low magnesium increases the risk of benign prostatic hyperplasia.
Vitamin D deficiency may be a marker of BPH.
In a study of BPH accompanied with metabolic syndrome, rats were treated with green tea extract. After 12 weeks, it significantly decreased the levels of glucose, total cholesterol, triglyceride, IGFs, and inflammatory cytokines, normalized the activities of antioxidant enzymes, as well as increased the prostatic expression of IGFBP-3 and PPARs. These results indicate that EGCG was able to exert anti-BPH activities in metabolic syndrome rats.
Helps lower excess estrogen levels.
Prevents inflammation found with this condition.

About the Author
Douglas C. Hall, M.D.
Dr. Douglas Hall, was born in Indianapolis, Indiana on Jan. 30, 1941. He received his BS and Doctor of Medicine at the University of Florida, training in obstetrics and gynecology. Dr. Hall has been in private practice since 1974 and currently has a large practice in Ocala, specializing in OB/GYN and Functional Medicine.

