Prior to menopause, the cells in the developing follicle produce a hormone called inhibin B, which in concert with estradiol, suppresses follicle stimulating hormone (FSH) from the pituitary (see Normal Menstrual Cycle). With decreasing numbers of normal follicles, there is inadequate production of inhibin B and estradiol and FSH will increase. Elevated FSH is an indicator of menopause.
Perimenopause precedes menopause by 2-8 years (average is 5 years). There are increasing symptoms, irregular menses and declining fertility. FSH will be elevated on day 3 of the follicular cycle. Many other conditions will present with similar symptoms, including insulin resistance, hypothyroidism, neurotransmitter abnormalities and depression. It is essential that women be evaluated for these conditions prior to making a diagnosis of perimenopause.
Perimenopause may be associated with hot flashes, mood swings, sleep disturbances, breast pain, breast enlargement, fatigue, headaches including migraines, and increasing flow and duration of menses. See Figure 1.
Menopause was once described as, “The ovaries, after long years of service, have not the ability of retiring in graceful old age, but become irritated, transmit their irritation to the abdominal ganglia, which in turn transmit the irritation to the brain, producing disturbances in the cerebral tissue exhibiting themselves in extreme nervousness or in an outburst of actual insanity.” (AM Farnham, Uterine Disease as a factor in the production of insanity. Alienist Neurologica 1887)
Menopause is the end of reproductive life. It can be a result of natural aging, surgical menopause where the ovaries are removed or chemotherapy. It occurs at age 40 in only 1% of the population and not until age 55 in 5% of the population. Several factors may affect the age at which menopause occurs, including tobacco use, medications, substance abuse, metabolic abnormalities, education and body mass index. The use of birth control pills in the past, race, height and number of children do not appear to have an effect on the age of onset.
Menopause Symptoms
There are many symptoms and metabolic changes associated with menopause. See Figure 2. Hot flashes are the common complaint. They have been described as ”sudden onset of reddening of the skin over the head, neck, and chest accompanied by a feeling of intense body heat and sometimes concluded by profuse perspiration.”
Hot flashes may last for a few seconds to minutes. They may occur frequently, more often at night and during times of stress, and are more common in overweight women. They usually last 1 to 2 years, but 25% of menopausal women will have them for more than 5 years. The metabolic changes associated with menopause can have far-reaching implications, including increased risk of metabolic syndrome, coronary artery disease, osteoporosis, Alzheimer’s, abnormal lipids, vaginal and urogenital atrophy, painful intercourse, recurrent urinary infections, decreased libido, depression, and painful intercourse, just to name few.

Managing Hot Flashes — Focus on Hormones
There are various therapies to manage hot flashes such as SSRIs (Paxil, Prozac) and SNRI (Effexor); Gabapentin (a nerve pain medication and anticonvulsant); and Clonidine (an antihypertensive and sedative). All of these have potential side effects. Will they decrease the risk of osteoporosis, vaginal atrophy, painful intercourse, heart disease and metabolic syndrome? If you have a flat tire, should you put air in the tire or take out the nail, repair the tire, and then put air in the tire? The concept is the same; the goal is to treat the cause in a safe and efficient manner.
Remember, hot flashes are not the result of a Prozac deficiency. The cause is a lack of hormones or a hormone imbalance. But each woman is different. Healthcare providers must determine through testing what each patient’s deficiencies or imbalances are before any therapy is initiated. They must also have knowledge of what affects hormone metabolism in order for their prescribed therapy to be safe and effective. For example, look at Figure 3.
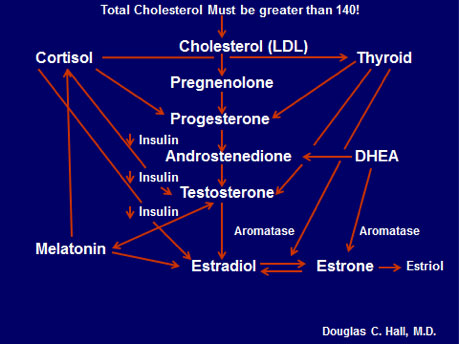
The hormones are in the middle, but look what affects them: thyroid, cortisol (which also affects thyroid), DHEA, melatonin and insulin. If any one of these is not functioning properly, it may alter the prescribed hormone therapy in an adverse manner.
Here is one example. Let’s say a woman has elevated insulin levels, but the healthcare professional prescribing the hormone therapy is unaware of that. A hormone prescription is written for estradiol, estriol, progesterone, DHEA and testosterone. This begins a potentially bad chain reaction, starting with aromatase, the enzyme that converts testosterone to estradiol, the most potent estrogen, and DHEA to estrone. This enzyme is increased by many factors, including increased insulin, low thyroid and abnormal cortisol. Androstendione and testosterone are increased by insulin and insulin increases aromatase, which converts them to the potent estradiol. To make matters worse, DHEA converts to estrone and that also metabolizes to estradiol. This woman is now at high risk for estrogen-dependent cancers, including breast and colon. The moral of the story: healthcare professionals who have extensive knowledge of hormone metabolism and biochemical pathways should be the only ones prescribing hormone therapy.
Hormones must be metabolized out of the body. There are three major pathways, with genetics and nutrition playing a major role in which pathway is selected. Look at Figure 4. It may look complicated, but believe me this is very simple.
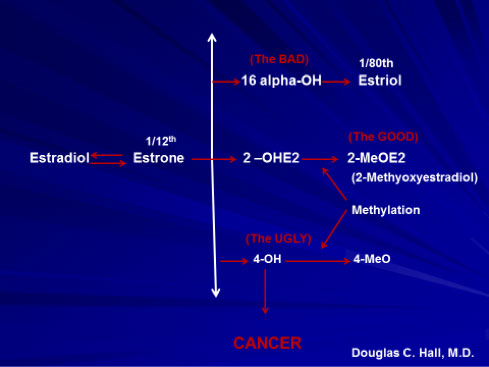
Estradiol and estrone can be metabolized through three different pathways: the 16 (the BAD), the 2 (the GOOD) or the 4 (the UGLY). Look at the potential benefits of being metabolized through the 2 pathway in Figure 5.
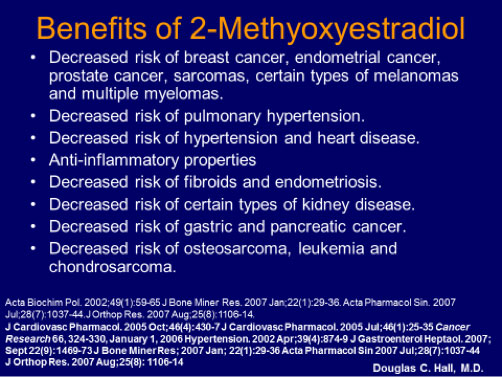
That is pretty impressive, but let’s take it one step further. Look at Figure 6.
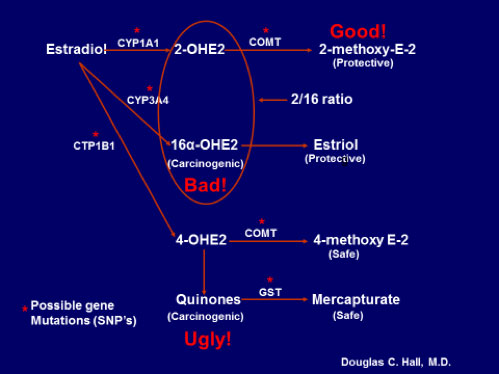
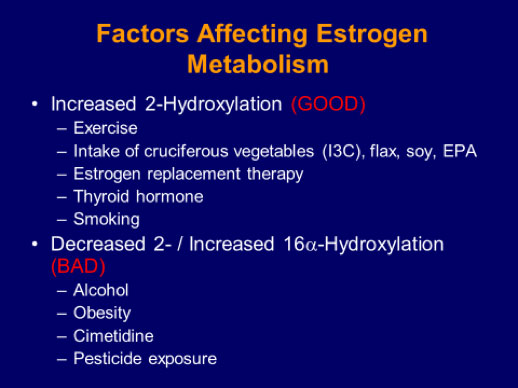
A number of possible gene mutations can affect how the hormones are metabolized. It is important to determine which mutations a woman has before prescribing hormone replacement therapy. The goal is to increase the 2 pathway. Look at what factors a woman can control that increase or decrease that pathway in Figure 7.
To go from the 2 Hydroxy to the 2 Methyoxy requires a chemical reaction called methylation and an enzyme called COMT, as depicted in Figure 8.
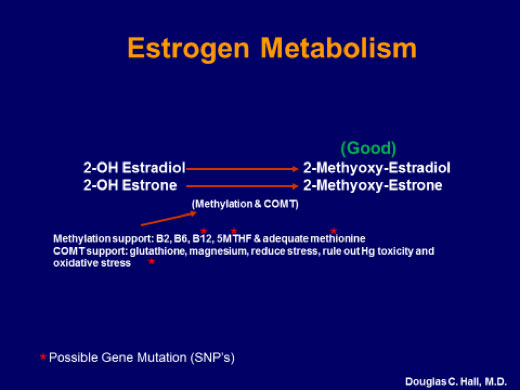
Methylation and COMT require B2, B6, B12, 5MTHF, adequate methionine, glutathione and magnesium. For optimal hormone metabolism, a micronutrient analysis is quintessential.
All hormones are fat-soluble; they will not dissolve in the blood until they are made water-soluble in the liver. In phase one of liver detoxification, hormones are made water-soluble. This involves numerous chemical reactions that require the following nutrients: Riboflavin (Vit B2), Niacin (Vit B3), Pyridoxine (Vit B6), 5-MTHF, Vitamin B12, Glutathione, Branched-chain amino acids and Flavonoids.
In phase 2 of liver detoxification, chemical reactions occur in which the hormones bind to certain chemicals and are excreted in the urine or stool. Nutrients required are Glycine, Taurine, Glutamine, N-acetylcysteine, Cysteine, Methionine and Phospholipids.
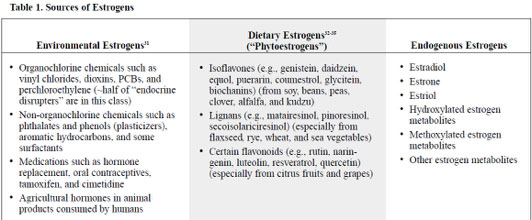
If any of the phase 1 or phase 2 nutrients are deficient, the hormones will not be detoxified in an efficient manner, which may result in an adverse health event. Keep in mind that the liver is also processing other chemicals such as end products of metabolism, bacterial endotoxins, exotoxins, drugs, chemicals, agricultural changes, food additives, and household pollutants/contaminants. Table 1 lists the various sources of estrogen the liver must process.
Copyright © 2001 by Advanced Nutrition Publications, Inc.
Nutrition and Estrogen Metabolism
When phase 1 and phase 2 are in balance, the partially detoxed chemicals pass on to phase 2 for further detoxification. If phase 1 detoxification exceeds phase 2, toxins will accumulate and cause tissue damage.
Glucuronidation is one of the key phase 2 liver detoxification pathways for estrogens and other toxins. Glucuronic acid is conjugated with estrogen to facilitate its elimination from the body. Unfortunately, some intestinal bacteria (most pathogenic) possess an enzyme, beta-glucuronidase, that uncouples the bond between excreted estrogen and glucuronic acid in the large intestines, allowing estrogen to reenter circulation (enterohepatic recirculation). Not surprising is the finding that excess beta-glucuronidase activity is associated with an increased cancer risk, including breast cancer. The activity of beta-glucuronidase is increased when the diet is high in fat and low in fiber, and can be reduced by establishing a proper bacterial flora by eating a diet high in plant foods and supplementing with “friendly bacteria” Lactobacillus acidophilus and Bifidobacterium infantis. It can also be resolved by taking calcium-d-glucarate. (Lett Appl Microbiol 1966;22(4):271-74)
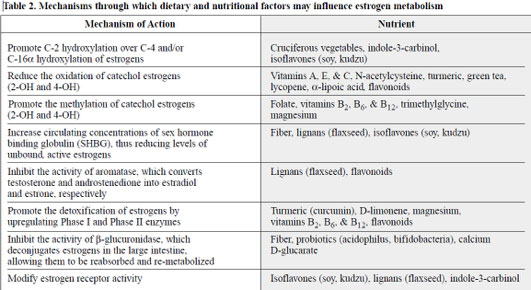
A summary of mechanisms through which dietary and nutritional factors may influence estrogen metabolism is listed in Table 2.
Copyright © 2001 by Advanced Nutrition Publications, Inc.
Benefits of Bioidentical Hormone Replacement Therapy
Used correctly, bioidentical hormone replacement therapy (BHRT) restores balance and relieves symptoms such as:
- PMS
- Hot flashes
- Mood swings
- Irritability
- Insomnia
- Loss of sex drive
- Vaginal dryness and painful intercourse
- Dry skin
- Sagging breasts
- Tender breasts
- Depression
- Brain fog
- Memory lapses
- Lack of energy
- Depression
- Anxiety
It can also lessen a woman’s risk of suffering from a number of health conditions:
- 50% less risk of stroke and heart attack
- 50% less risk of broken bones from osteoporosis
- 80% less risk of Alzheimer’s
- 40% less risk of osteoarthritis
- 40% less risk of periodontal disease and tooth loss
- 30% less risk of colon cancer
Women using BHRT also experience fewer wrinkles and other visible signs of aging skin. Studies show that women who use BHRT look younger than their age, and women who do not use BHRT after menopause look older than their age. (https://www.holtorfmed.com/hormonal-imbalance-for-women/)
Treatment with BHRT
Before any treatment is initiated, a complete evaluation should be completed as described above. There are numerous estrogen preparations on the market, but ideally balanced therapy including estrogen, progesterone, DHEA, and testosterone should be considered based on a woman’s evaluation and symptoms.
Estrogen Preparations
Premarin – conjugated equine estrogens comprised mostly of estrone sulfate; 10 estrogens total with doses of 1.25 mg, 0.625 mg, 0.45 mg, and 0.3 mg
Cenestin – conjugated estrogens derived from plant source, very similar to premarin and containing 9 estrogens
Enjuvia – also conjugated estrogens derived from plant sources
Estratab, Menest – esterified estrogens derived from plant sources that result in serum estradiol and estrone levels similar to premarin
Ogen – naturally derived, purified estrone sulfate
Estrace – micronized preparation of estradiol
Oral Combination Preparations
Prempro – a combination of premarin and progestin
FemHrt – ethinyl estradiol (potent synthetic estrogen used primarily in OCPs) with norethindrone acetate; doses = 2.5 mcg/0.5 mg and 5 mcg/1 mg
Angeliq – 1 mg estradiol/ 0.5 mg drospirenone
Activella – 1 mg estradiol/ 0.5mg norethindrone
Transdermal Estrogen
Contains 17-beta estradiol
Doses range from 25 to 100 mcg/day
50 mcg/day is equivalent to 0.625 mg of conjugated estrogen
Vivelle-dot or Minivelle
0.025, 0.0375, 0.05, 0.075, 0.1/day patch
Menostar
Ultra low dose, 14 mcg/day
Addition of progesterone may be two 14-day cycles/year
Combined Patches
Combipatch
50 mcg/day 17 beta estradiol
0.14 or 0.25 mg/day norethindrone acetate
Climara Pro
45 mcg/day 17 beta estradiol
0.15 mg levonorgestrel
Topical Estradiol Preparations
Estrasorb (estradiol emulsion)
0.05 mg/day estradiol
EstroGel
0.75 mg/day
Divigel
1 mg estradiol/g (apply 0.25 g)
Elestrin
0.87 g gel provides 0.52 mg estradiol
Evamist
1.53 mg/spray
Progesterone Preparations
Prometrium – natural micronized progesterone
Medroxyprogesterone
Drosperinone
Megestrol acetate
Testosterone derivatives – have some weak androgenic actions
Norethindrone
Norgestrel
Levonorgestrel
Compounded Preparations
These preparations usually contain estradiol and estriol in a 50/50 or 80/20 ratio, in combination with natural progesterone, DHEA, and testosterone. Healthcare providers determine the strength of each component based on each woman’s needs. They can be compounded in an oral pill; applied to the cheek in the mouth; or taken via a transdermal cream usually applied twice a day, Monday through Friday, to a fatty area of the body such as the forearm or inner thigh.
The advantage of the transdermal cream is that it bypasses the liver. Transdermal creams do not increase the risk of blood clot formation. Follow-up salivary testing is required for women using transdermal creams and buccal applications, while blood tests can be used for follow-up for those taking an oral preparation. The risks of taking an oral preparation, as per Pamela W. Smith, M.D., MPH, MS, are:
- Increased blood pressure
- Increased triglycerides
- Increased estrone
- Causes gallstones
- Elevates liver enzymes
- Increases SHBG (decreases testosterone)
- Interrupts tryptophan metabolism and consequently serotonin metabolism
- Lowers growth hormone
- Increases prothrombic effects
- Increases CRP
- Increases carbohydrate cravings
Hormone Pellets
Hormone pellets are by far the most efficient means to deliver bioidentical estrogen and testosterone therapy. Hormone replacement therapy using pellets has been used in the U.S., Europe and Australia since 1938. More than 70 years of research has illustrated the benefits of pellet implants in administering hormones in men and women. Pellet implants deliver consistent, physiologic levels of hormone, dosing that has shown to maintain and improve bone density. Pellet implants bypass the liver and don’t negatively impact clotting factors, blood pressure, lipid levels, glucose, or liver function.
Pellets implants have consistently been shown to improve:
- Cardiovascular health
- Sex drive and libido
- Headaches and migraines
- Hot flashes
- Mood and depression
- Joint aches and pains
- Irritability
- Anxiety
- Physical fatigue
- Memory loss
- Bladder problems
- Vaginal dryness (Glaser 09)
Pellet insertion is a relatively simple in-office procedure done under local anesthesia. The pellets are inserted in the fatty tissue under the skin either in the lower abdomen or the upper buttocks through a very small incision. The incision is closed using sterile-tape strips. Patients cannot feel the implants under the skin. Implants placed under the skin consistently release small, physiologic doses of hormones that have been shown to have many benefits.
Fused pellet implants typically last between 4-6 months, depending on how rapidly the hormones are metabolized. After insertion of the pellets, vigorous physical activity should be avoided for 2-3 days. Some patients begin to feel symptom relief within 48 hours, while others may take up to two weeks to notice a marked difference. The pellets do not need to be removed. They are completely dissolved by the body.
The most efficient means of monitoring the prescribed hormone therapy, regardless of whether it is oral, sublingual, transdermal, vaginal or anal, and pellets, patches, or injections, is through dried urine testing, DUTCH (Dried Urine Test for Comprehensive Hormones).
Recommended Supplements to Treat Menopause:
Supports healthy estrogen metabolism in females and males.
Higher levels of vitamin C decrease the risk of breast cancer.
Methylation is essential for the proper metabolism of estrogen.
Vitamin D deficiency is common among reproductive-aged women and has a role in female reproduction. Long-term use of calcium and vitamin D appears to confer a reduction that may be substantial in the risk of hip fracture among postmenopausal women.
Xeno Detox is a comprehensive formula designed to support Phase I and II liver detoxification of environmental pollutants, endocrine disruptors, estrogen metabolites, xenoestrogens, and other toxins. Supports healthy estrogen metabolism.
You need iodine for the thyroid and other glands in the endocrine system. The breasts, salivary glands and ovaries depend on iodine. For example, proper functioning of the thyroid is needed to make progesterone and detoxify, etc.
The risk of a hip fracture is equivalent to the COMBINED risk of developing breast, uterine and ovarian cancer. Osteo MK-7 uses an array of complementary, well-researched nutrients to build and maintain bone, especially during perimenopause and menopause.
The experimental data provides strong evidence to support the anticancer activities of δ-tocopherol, γ-tocopherol, and the natural tocopherol mixture rich in γ-tocopherol, γ-TmT, over α-tocopherol.
Supports healthy endocrine function. Consumption of green tea decreases the risk of breast cancer and uterine cancer.
Abnormal microbiome may produce an enzyme called beta-glucuronidase, which, recycles estrogens and increases the risk of estrogen-related cancers.
Magnesium deficiency is a contributing factor to anxiety and panic attacks during perimenopause and menopause.

About the Author
Douglas C. Hall, M.D.
Dr. Douglas Hall, was born in Indianapolis, Indiana on Jan. 30, 1941. He received his BS and Doctor of Medicine at the University of Florida, training in obstetrics and gynecology. Dr. Hall has been in private practice since 1974 and currently has a large practice in Ocala, specializing in OB/GYN and Functional Medicine.

